The Revenue Cycle Blog
Filter By
- ABA Therapy Billing
- AI in Medical Billing
- AI in Revenue Cycle
- Accounts Receivable Management
- Accounts Receivable Mangement
- Allergy and Immunology Billing Services
- Anesthesia Billing Services
- Back Office Revenue Cycle
- Bariatric Surgery Billing
- Billing For Physician Practice and Medical Groups
- Billing for Physician Practices and Medical Groups
- Blog
- COVID-19 Billing
- CPT Codes
- Cardiology Billing Services
- Charge Capture Services
- Charge Entry - Medical Billing
- Charge Entry Services
- Clinical Documentation Improvement - CDI
- Clinical Documentation Integrity
- Company News
- Credit Balance Services
- DME Billing Services
- Denial Management - Medical Billing
- Dermatology Billing Services
- E&M
- Electronic Health Records
- Eligibility and Benefits Verification Services
- Emergency Department Billing Services
- FAQs
- G Code
- Gastroenterology Billing Services
- General Surgery Billing Services
- HCC Coding
- HCC Coding Services
- HCPCS
- Healthcare Collections
- Hospitals
- Internal Medicine Billing Services
- Medical Billing Company
- Medical Billing Services
- Medical Billing Services in California
- Medical Billing Services in Texas
- Medical Claim Submission
- Medical Coding Services
- Mental health Billing Services
- Mid Cycle in Revenue Cycle
- Modifiers in Medical Coding
- Neonatal Billing Services
- Neurology Billing Services
Revenue per Encounter – The top revenue cycle metric
Revenue per encounter can be defined and computed by dividing net collections by the total number of patient visits in a given month. This metric can provide a quick view of the health of your revenue cycle. In this whitepaper from Medical Billing Wholesalers, learn more about how to calculate and increase Revenue per encounter.
Shifting the Focus from Denial Management to Denial Prevention
The adage, “Prevention is better than cure”, does apply to Claim Denials as well. An effective denial prevention program requires an iterative process that includes identification of root cause, finding solutions to prevent the issue from recurring in the future, the institutionalization of these procedures through updates to standard operating procedures, and training the staff on these practices. In this whitepaper from Medical Billing Wholesalers, we bring you a few steps that you can take to prevent denials.
Improving Collections by using the right CPT Codes for Prolonged Service
While the application of prolonged service codes may be fairly simple, very few codes cause more confusion than prolonged service codes. It may be noted that prolonged service codes can be used for outpatient procedures as well as for inpatient care. These codes are typically used to bill for services that significantly exceed the standard time a physician takes while providing care. These may include face-to-face services as well as non-face-to-face services.
While prolonged service coding issues are highlighted in this case study, the principles of educating physicians and clinical staff is applicable for all cases where coding denials are high.
Best Practices in filing Physician Assistant Claim enable Recovery of over $80 K in out-of-network claims
Recovering claim dues from payers for physician assistance claims requires intricate knowledge of payer-specific guidelines. Medical Billing Wholesalers’ denials research team helped the client identify and resolve out-of-network claims.
With a focus on recovering denials of PA claims from UHC and Oxford, we rebilled the claims after adhering to the payer-specific guidelines and were able to recover over $80K of A/R, while reducing the monthly denials from 73 to 11.
Correct Coding and Re-submission of Pain Management Claims help Recover $300K of A/R Backlog
Standardized billing and coding practices for Spinal Cord Stimulator (SCS) Procedure Code 63650 reduce medical necessity denials and help collect 281 claims valued over $ 300K in 2 years. The Customer saw over 36% improvement in Collections, as much as 75% reduction in old AR over 61 days, and reduction of denied SCS claims from 68 to 8 over a 7 month period.
Medical Coding & Best Practices Guide - Podiatry
Podiatry billing can be complicated in many ways, beginning the need to determine and prove the medical necessity of the treatment, to the coding nuances. It demands meticulous use of modifiers and an understanding of coding for inclusive procedures. In this guide, Medical Billing Wholesalers bring you the guidelines & best practices to be followed to increase collections of your Podiatry practice.
Denial Management Infographic
Get the statistics for claim denials and strategies for preventing them in this Denial Management infographic from Medical Billing Wholesalers.
Reimbursements for COVID-19 Treatments & Testing of Uninsured Individuals
As with all other industries, healthcare providers are facing financial challenges stemming from COVID-19. Getting reimbursements for COVID-19 treatments of uninsured individuals is complicated & requires healthcare providers to stay up to date with the nuances of the HRSA program for the uninsured. In this article we provide a consolidated view of everything one should know about the HRSA program for COVID-19 treatments of the uninsured.
How to Arrest Revenue Leakage in Medical Billing?
Inefficiency & carelessness in the revenue cycle stages can cause revenue leakage, which if undetected, could result in the loss of thousands of dollars. In this whitepaper, we bring you 10 things that you can implement to reduce revenue leakage in your practice. These best practices will help you improve revenue and reduce your costs.
The Increasing Acceptance of Telemedicine for Care Delivery in the Post COVID-19 Era
Telemedicine is gaining increasing acceptance as a direct consequence of the Coronavirus outbreak. The bigger question is if telemedicine will continue and possibly even grow post-COVID-19 or is this just a passing phase that has gained popularity out of necessity and will wane off. In this article, MBW brings you a list of reasons why Telemedicine is the new normal.
4 Reasons for Physical Therapy Claim Denials and Solutions
Denied claims are the type of claims that were received and processed by the insurance payer and a negative determination was made. It is no wonder that in Physical Therapy there are a greater number of denied claims compared to any other specialty. Read more about reasons for claim denials in Physical Therapy and ways to rectify them.
Mastering Physical Therapy Billing - Codes & Terminologies You should Know
Medical Codes and Terminologies are two essential things that a Physical Therapist should learn about. The Medical codes define the diagnoses, treatment, procedures, and medication used through the alphanumeric ICD-10 Coding System. In this article, we provide you a view of the physical therapy codes and terminologies.
Revenue Cycle in the Times of COVID-19 – Creating a Sustainable Financial Future
COVID-19 updates by the regulators are across the news today. With many physician practices choosing to operate remotely, and reduced patient visits to the outpatient department, the financial health of healthcare providers is now reeling under the shock of COVID-19. MBW brings you some of the areas that financial administrators working at healthcare provider entities must focus on to stabilize financial operations and restore normalcy.
World Health Day 2020 – Saluting the undying spirit and commitment of Nurses and Midwives
Medical Billing Wholesalers salutes the undying commitment of the medical fraternity across the world. We see our role as helping the healthcare systems improve the economics of healthcare enables caregivers to focus on what they do best, deliver high-quality care. On this day, renew and reaffirm our commitment to helping the medical community reduce administrative costs, and improve care delivery.
New CPT Code Released to report laboratory testing services that diagnose the presence of the novel Corona Virus
The unique CPT code will be used to report laboratory testing services that diagnose the presence of the novel coronavirus. This will help provide the data for analytics as testing to identify the incidence of the virus continues across the United States.
Revisiting the Basics: Understanding Medical Coding - Importance and Career Opportunities
Medical Coding is a key element of the revenue cycle and drives the communication between healthcare providers and insurers. In this article, we talk about the importance of medical coding and the career opportunities the field presents
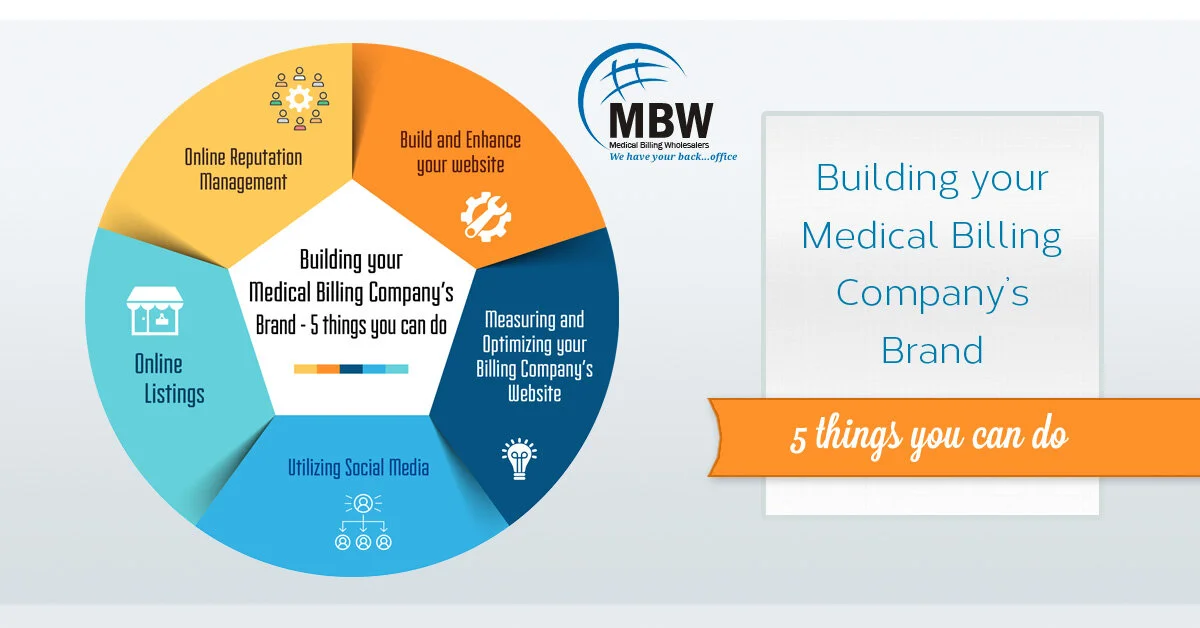
Building your Medical Billing Company’s Brand – 5 things you can do
As Medical Billing Company Owners and Managers, you need to build and manage your company's brand, build the online presence, and manage your reputation. Medical Billing Wholesalers brings you a comprehensive guide on building your company's brand and digital presence.
Improving Days in A/R: A Best Practices Guide to Optimize Your Revenue Cycle
Improving days in A/R to MGMA benchmark of fewer than 40 days requires a comprehensive relook at the entire revenue cycle and concerted efforts to improve. In this article, we bring you insights on how to reduce the number of days in AR.
Revenue Cycle Trends for 2020 and Beyond
With headwinds coming from falling reimbursements and the rise of national-level aggregators, the times are tough for medical billing companies.
In this whitepaper, we look at some of the trends and what medical billing companies need to do to survive and thrive in 2020 and beyond.